Fake Doctor Exposed? The Gustavo Quirs Licona Case
Would you trust a self-proclaimed expert with your health, especially when evidence suggests they might not be who they claim to be? The alarming rise of medical professionals operating outside their certified expertise demands urgent attention, potentially jeopardizing patient safety and eroding public trust in the healthcare system.
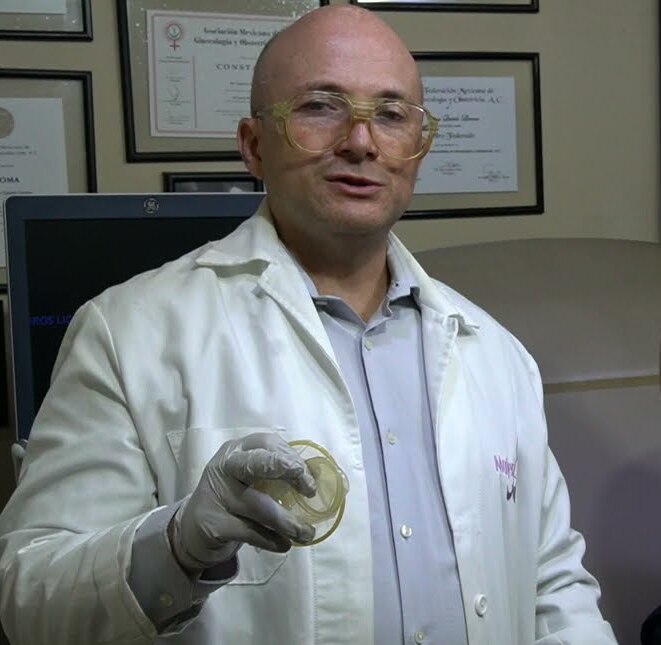
The case of Gustavo Quirs Licona has recently surfaced, raising serious questions about medical credentials and the potential for professional misrepresentation. Social media has become a battleground where concerns regarding Licona's qualifications have been amplified, specifically concerning his claims of being a gynecologist. While presenting himself as such online, scrutiny reveals inconsistencies between his public persona and official records.
The heart of the matter lies in the apparent discrepancy between Licona's professional self-promotion and his registered credentials. The National Registry of Professionals indicates that Gustavo Quirs Licona is registered as a medical surgeon, a qualification that, while respectable, does not automatically translate into expertise in gynecology. The absence of documented specialization in gynecology raises concerns about the validity of his claims and the potential risks patients might face if they seek his services under the impression that he is a fully qualified gynecologist.
- How Old Is Traci Braxtons Son Uncovering The Details
- Unveiling Sams Reallife Companion From General Hospital
| Category | Information |
|---|---|
| Full Name | Gustavo Quirs Licona |
| Profession Claimed | Gynecologist |
| Registered Profession | Medical Surgeon |
| Social Media Presence | TikTok: @dr.gustavo.quiros (31.9k Likes, 9427 Followers) |
| Concerns Raised | Potential misrepresentation of qualifications; practicing outside of certified expertise. |
| Source of Information | National Registry of Professionals, Social Media (TikTok), Online accusations by "charlatanes mdicos" |
| Reference Website | National Registry of Professionals (Mexico) |
The implications of this case extend beyond a simple matter of misrepresentation. It highlights the increasing importance of verifying the credentials of medical professionals, especially in an era where information and misinformation spreads rapidly through online channels. Social media, while offering a platform for doctors to connect with patients, also presents opportunities for individuals to promote themselves without adequate oversight, potentially leading to the dissemination of misleading information about their qualifications and expertise.
Adding to the controversy, Licona's online activity reveals a history as a traumatologist who also advertises as a gynecologist. This professional duality raises further questions regarding his training and experience in gynecology. While a background in traumatology may provide valuable medical knowledge, it does not necessarily equip an individual with the specific skills and expertise required to provide safe and effective gynecological care.
The proliferation of social media has undoubtedly changed the landscape of healthcare marketing, providing medical professionals with unprecedented opportunities to reach potential patients. However, this increased accessibility also comes with increased responsibility. Doctors who use social media to promote their services must be transparent about their qualifications and expertise, and they must avoid making claims that could mislead or deceive patients.
- Unveiling The Luxurious Abode Of Ryan Reynolds And Blake Lively
- All About Homer James Gere Early Life Career And More
The core problem is not just about one individual; it's about the system that permits this kind of potential deception. Existing regulatory bodies often struggle to keep pace with the rapid evolution of online marketing and self-promotion. The lack of robust mechanisms for verifying credentials and monitoring online claims creates a fertile ground for individuals to misrepresent themselves and potentially harm unsuspecting patients.
Consider the hypothetical scenario of a patient seeking gynecological care based solely on Licona's online presence, unaware that his specialization in this area is not formally recognized. This patient might be deprived of the specialized care they need and deserve, potentially leading to misdiagnosis, inappropriate treatment, or even serious health complications. The responsibility for preventing such scenarios falls not only on individual practitioners but also on regulatory bodies and the public at large.
The medical profession has always rested on a foundation of trust and accountability. Patients place their well-being in the hands of doctors, trusting that they possess the necessary qualifications and expertise to provide competent care. When that trust is violated, the consequences can be devastating, not only for individual patients but also for the integrity of the entire healthcare system.
While Licona's case is attracting attention, it is essential to remember that this is not an isolated incident. Throughout the world, there have been instances of medical professionals practicing outside their certified expertise, leading to severe harm for patients. These cases serve as a sobering reminder of the importance of vigilance and the need for ongoing efforts to strengthen the regulatory framework governing the medical profession.
The challenge lies in creating a system that is both effective in preventing medical misrepresentation and respectful of the rights of legitimate practitioners. This requires a multi-faceted approach that involves strengthening credentialing processes, enhancing monitoring of online activity, and educating the public about the importance of verifying medical qualifications.
One potential solution is to establish a centralized online database of medical professionals that is accessible to the public. This database would provide detailed information about each doctor's qualifications, including their areas of specialization, board certifications, and any disciplinary actions taken against them. Patients could then easily verify a doctor's credentials before seeking their services, empowering them to make informed decisions about their healthcare.
Another key element is enhancing the monitoring of online activity. Regulatory bodies need to develop sophisticated tools to identify medical professionals who are making false or misleading claims about their qualifications. This could involve using artificial intelligence to scan social media platforms and websites for potentially fraudulent content. When such content is identified, regulatory bodies should take swift action to investigate and, if necessary, impose sanctions.
In addition to strengthening credentialing and monitoring, it is also essential to educate the public about the importance of verifying medical qualifications. Patients need to be aware that not everything they see online is accurate, and that they should always take steps to confirm a doctor's credentials before seeking their services. This could involve launching public awareness campaigns that highlight the risks of medical misrepresentation and provide patients with the resources they need to verify a doctor's qualifications.
The medical community also has a role to play in preventing medical misrepresentation. Doctors should be encouraged to report suspected cases of fraud or misrepresentation to the appropriate authorities. They should also be mindful of their own online presence and avoid making claims that could mislead or deceive patients.
Ultimately, preventing medical misrepresentation requires a collaborative effort involving regulatory bodies, the medical community, and the public at large. By working together, we can create a healthcare system that is built on trust, transparency, and accountability, ensuring that patients receive the safe and effective care they deserve.
The case of Gustavo Quirs Licona serves as a stark warning about the dangers of unchecked self-promotion and the potential for patients to be misled by individuals posing as qualified medical professionals. By strengthening credentialing processes, enhancing monitoring of online activity, and educating the public about the importance of verifying medical qualifications, we can take steps to protect patients and preserve the integrity of the healthcare system.
Consider, for instance, the ramifications of unqualified individuals performing procedures like colposcopies or IUD insertions, procedures requiring a nuanced understanding of anatomy and potential complications. The absence of proper training could lead to cervical damage, infections, or even perforation of the uterus, consequences that can have long-term repercussions for a woman's reproductive health.
Furthermore, the lack of specialized knowledge can manifest in misdiagnoses or delayed diagnoses. A self-proclaimed gynecologist without proper training might overlook subtle signs of cervical cancer or fail to identify hormonal imbalances, leading to delayed treatment and potentially worsening outcomes. The ripple effects of such errors can be devastating, impacting not only the patient's physical health but also their emotional well-being and quality of life.
The issue also extends to the realm of prenatal care. A qualified obstetrician is trained to identify and manage potential complications during pregnancy, such as pre-eclampsia, gestational diabetes, or ectopic pregnancies. An unqualified individual might lack the knowledge and skills to recognize these warning signs, putting both the mother and the baby at risk.
Another critical area is the management of menopause. Qualified gynecologists are equipped to provide personalized care to women experiencing menopause, including hormone replacement therapy and lifestyle recommendations. An unqualified individual might prescribe inappropriate treatments or fail to address underlying health conditions, potentially exacerbating symptoms and increasing the risk of long-term health problems.
The potential for harm extends beyond individual procedures and treatments. An unqualified individual might also lack the knowledge and skills to provide comprehensive sexual and reproductive health education. This can have serious consequences for public health, as it can lead to increased rates of unintended pregnancies, sexually transmitted infections, and other health problems.
Beyond the clinical aspects, there's the ethical dimension. A legitimate medical professional adheres to a strict code of conduct, prioritizing patient well-being above all else. This includes obtaining informed consent, maintaining confidentiality, and avoiding conflicts of interest. An unqualified individual might not be aware of these ethical obligations or might choose to disregard them, potentially exploiting vulnerable patients for personal gain.
The financial implications are also significant. Patients who receive substandard care from unqualified individuals may incur significant medical expenses to correct the damage caused. They may also lose time from work and experience emotional distress, adding to the overall cost of the experience.
The increasing reliance on telemedicine and online consultations further complicates the issue. While telemedicine can provide convenient access to healthcare, it also makes it easier for unqualified individuals to practice medicine across state lines or even internationally. Regulatory bodies need to develop effective mechanisms to oversee telemedicine practices and ensure that patients receive care from qualified professionals, regardless of their location.
The challenge is not only about identifying and prosecuting unqualified individuals but also about creating a culture of accountability within the medical profession. Medical schools and training programs need to emphasize the importance of ethical conduct and the potential consequences of practicing outside one's area of expertise. Hospitals and clinics need to implement robust credentialing processes to ensure that all medical professionals are properly qualified and licensed.
In addition to strengthening the regulatory framework, there is also a need for greater collaboration between regulatory bodies, law enforcement agencies, and social media platforms. These entities need to work together to identify and remove fraudulent medical content from the internet and to bring unqualified individuals to justice.
The solution is not to stifle the use of social media by medical professionals but rather to promote responsible and ethical online behavior. Medical organizations can develop guidelines for social media use that address issues such as truthfulness, transparency, and patient privacy. They can also provide training to their members on how to use social media effectively and ethically.
Ultimately, the responsibility for protecting patients from medical misrepresentation lies with each and every one of us. Patients need to be informed consumers of healthcare, asking questions, verifying credentials, and reporting suspected cases of fraud. Medical professionals need to be vigilant in upholding ethical standards and reporting colleagues who are practicing outside their area of expertise. Regulatory bodies need to be proactive in enforcing the laws and regulations governing the medical profession.
The proliferation of misinformation in the digital age necessitates a proactive stance from both patients and regulatory bodies. Before entrusting their health to any professional, individuals must diligently verify credentials, scrutinize online testimonials, and seek second opinions when necessary. Furthermore, regulatory agencies must enhance their surveillance capabilities to detect and swiftly address instances of medical misrepresentation, ensuring that the public is shielded from potential harm.
The long-term consequences of failing to address medical misrepresentation are dire. A decline in public trust in the healthcare system could lead to reduced utilization of essential medical services, increased rates of preventable diseases, and a widening gap in health equity. It is therefore imperative that we take decisive action to protect patients and preserve the integrity of the medical profession.
The case of Gustavo Quirs Licona is a symptom of a larger problem that requires a comprehensive and coordinated response. By strengthening credentialing, enhancing monitoring, educating the public, and fostering a culture of accountability, we can create a healthcare system that is worthy of the public's trust.
- Unveiling The Luxurious Abode Of Ryan Reynolds And Blake Lively
- The Stanbury Dynasty Unraveling Caroline Stanburys Ancestry
Dr. Gustavo Quirós Licona Contact for Inquiries, Audience Analysis
Post from Dr. Gustavo Quirós Licona

Gustavo Quirós Licona El DOCTOR más OSCURO y perverso de YouTube YouTube